Modern nuclear medicine at Helios - an interview with Prof. Dr. med. Dresel
Nuclear medicine involves using radioactive substances for diagnostics and treatment. What is the difference between nuclear medicine, radiotherapy, and radiology? What is radionuclide therapy, and what approaches are currently the most promising? These are the topics of our conversation with Prof. Dr. med. Stefan Dresel, Chief Physician of the Nuclear Medicine Department of the Helios Hospital Berlin-Buch.
• There are so many questions regarding nuclear medicine, as people often don't understand the medical terms very well. So let's start with general questions. There are different names of your specialty that may appear both in Russian and German texts: nuclear medicine, radiotherapy, radiology, and radionuclide therapy. Are these synonyms? Or are there any particularities regarding the use of these terms?
This is a very important question as all these terms must be strictly distinguished. Radiology is medical imaging and should be clearly distinguished from nuclear medicine. Radiotherapy is another separate discipline with a totally different principle: radiotherapy involves external irradiation of patients. By using an accelerator, irradiation is being sent through the skin towards the tumor.
Thus, radiology and radiotherapy are separate areas of medicine that should be distinguished from nuclear medicine.
However, when we talk about radioactive substances that are put into a patient's body - usually in a form of intravenous injection, or procedures where patients inhale or swallow radioactive substances - then we are talking about radionuclide therapy. Radionuclide therapy is one part of nuclear medicine.
When we introduce radioactive substances into a patient's body for treatment purposes, it is called radionuclide therapy. Whether this method is deemed appropriate for treatment or diagnostics depends on the specific radioactive substance. We have substances that allow us to obtain excellent images and perform diagnostics — this is not therapy; but we also have other substances that we then use for treatment, i.e. radionuclide therapy.
-
What is the innovative factor of using Lutetium-177 for therapy? What type of irradiation is it? In which cases does this method prove to be effective?
Allow me to reach back a bit. In the field of nuclear medicine, we've gathered decades of experience using iodine-131 in radionuclide therapy for thyroid cancer patients. This is a classic treatment method that nearly all patients diagnosed with thyroid gland diseases are receiving. One of your next questions in this context was about Russia. We all know that in 1986 there was an incident at the nuclear power plant in Chernobyl, which led to the release of radioactive substances. As an aftereffect it could be seen that many inhabitants in the region around the nuclear power plant were diagnosed with thyroid cancer. All these patients received radionuclide therapy in addition to surgical treatment. For us, this is a common procedure, and it has been performed with iodine-131 for several decades now.
And then, about 10 years ago, they started to develop new substances with lutetium-177. First, such substances were developed for neuroendocrine tumors, such as so-called DOTATOC, and then, since about 6 years - the PSMA for the therapy of prostate carcinoma. The PSMA stands for prostate-specific membrane antigen, which binds directly to the tumor cell of the prostate carcinoma according to a lock-and-key principle. The PSMA docks onto the surface of the prostate carcinoma, binds tightly there, and is then transported into the cell. Attached to the PSMA is the lutetium-177, which is then also in the cell. The lutetium-177 is radioactive, it decays and thus destroys the tumor cell. This is the principle of highly selective therapy, because the substance binds exclusively to the tumor cell and can destroy it via the radioactive portion of lutetium-177. Importantly, the substance only affects the normal organ tissue to a very small extent and does not cause any damage. As I always say, this is a form of elegant therapy that one would like to see for other tumor diseases. There is nothing like this yet for other diseases, but work is currently being done on that. But for prostate carcinoma or for neuroendocrine tumors, there is precisely this therapy with which we can treat the tumor cells quite selectively.
-
Are there many hospitals in Germany that could also perform these therapies?
There are certainly some hospitals that do this. Helios Berlin-Buch was one of the first hospitals to do so. We have been working with these therapies for about 6 years now.
The PSMA substance was developed in Germany, in Heidelberg. The first therapies were also carried out there. We are certainly among the clinics that have been able to gain considerable experience there in recent years.
When we talk about the Lutetium PSMA therapy again, it is important that we do not take the decision about the therapy alone, but always in an interdisciplinary tumor board. We discuss the patient's case there and then together with the urologists, with the oncologists and the radiation therapists, to make the indication for the therapy. There are a variety of therapeutic options and substances for the therapy of prostate cancer and it is important to find a specific therapy for the patient at a certain point in time, also following the international guidelines. Lutetium-177 is an innovative new therapy that is very well tolerated and shows very good response rates.
-
You treat patients with thyroid cancer using radioiodine therapy. What is it all about? What are the results of this technique? Is it also effective in treating other types of cancer?
Radioiodine therapy is only effective for so-called differentiated thyroid carcinoma (papillary and follicular thyroid carcinomas). Here, with a few exceptions, it is customary and, according to international guidelines, also necessary that patients additionally receive the so-called adjuvant therapy before surgery, even if they do not have metastases, in order to provide additional safety for the future. This procedure works well in the case of thyroid carcinoma because in the human organism only the thyroid gland is able to specifically absorb iodine. All thyroid tumor diseases usually have this characteristic, therefore, in addition to surgery, we use radioiodine therapy to improve the prognosis of patients and also to safely eliminate all cells in the body that have to do with thyroid tissue. This is achieved with radioiodine therapy.
-
Germany is the third largest market for nuclear medicine in the world after the U.S. and Japan. You studied in the U.S. - could you tell us about the special features of treatment in Germany? What are the advantages? What are the differences?
The procedures mentioned, be it radioiodine therapy or procedures with lutetium, are also available in the USA. Radioiodine therapy in particular is intensively practiced there. Here in Germany, we offer radioiodine therapy not only for tumor diseases, but also for benign diseases of the thyroid gland. In the U.S., radioiodine therapy has a higher priority than here in Germany, because traditionally a lot of thyroid surgery is performed in Germany, more than is common worldwide.
In other countries and also in the U.S., radioiodine therapy is done for many diseases - even benign ones - whereas here in Germany patients are receiving surgery. So, this is a rather locally different procedure.
Let me come back to lutetium therapy. With PSMA, it is the case that it is not yet approved in the U.S. at the moment. The substance Lutetium PSMA is currently in the approval process, but approval has not yet been granted worldwide, both in the U.S. and in Europe. In Germany, we have the opportunity, based on our Medicines Act, to be able to use this substance even before it has been approved and to be able to treat patients with it within the framework of the introductory periods and the so-called "individual healing trial". This is something that is unique in the world. We offer this therapy in coordination with the authorities, although there is not yet a company commercially available to buy the substance. And that is our great advantage in Germany, that patients have access to the Lutetium PSMA therapy at this early stage and can benefit from it, although the substance is not yet available in other countries worldwide.
This is important for the patients, because this therapy shows a very good effect, and it is also good for us that we can participate in this modern procedure so early and have access to it.
I would like to mention at this point that just in June last year (2021), a large study was published, the so-called Vision Study, on the Lutetium PSMA therapy in prostate cancer in comparison to standard therapy. The study has shown very excellent results and has been so well accepted internationally that we expect that after this study, international approval of the PSMA Lutetium-177 will also be granted in the near future. Even more important for the patients and for us as treating physicians is that what we see in our patients in terms of good therapy effects has also been confirmed in the published study (The New England Journal of Medicine).
-
Do you often encounter patients' fears and concerns about radiation? There are many myths about radiation therapy - for example, that it is only prescribed to people who are terminally ill, or that it causes radiation sickness. Do you deal with such myths in your work? How do you deal with them?
It is exactly like you've just said. We take a lot of time to talk to patients about these myths and to educate them about at which stage which therapy is the right one. It has to be mentioned in prostate cancer that there are also very effective other therapies, such as hormonal therapy or chemotherapy. In our work, we are of course initially guided by the international guidelines. That means that at the moment the established therapies have to be carried out first, such as anti-hormonal therapy, radiation therapy, chemotherapy or surgery. And only when these therapies no longer work, then the Lutetium PSMA therapy is used. In the course of prostate cancer there is a stage when the prostate cancer and the associated metastases become hormone-refractory and no longer respond to anti-hormonal therapy. Then usually another attempt at chemotherapy is made and if that is not successful, then Lutetium PSMA therapy is indicated. This is the procedure according to all available guidelines at the moment. This may change in the future, when the new therapies are only used when the already established and highly effective therapies are no longer successful. Whether the Lutetium PSMA therapy can possibly have an even better effect at an earlier stage, that is currently being investigated, we don't know yet. We still have to wait for these results.
There are individual patients who could not receive chemotherapy for other reasons or who did not persevere with anti-hormonal therapy. In these patients, there is experience of using PSMA therapy earlier with very good efficacy. However, this has not yet been investigated to a sufficient extent scientifically, so we will have to wait for future studies.
-
Which clinical pictures do you deal with most frequently in your specialist department? How does it usually work - do specialists from other fields refer their patients to you for diagnosis and treatment?
When we talk about the therapies, what we just listed is the thyroid carcinomas, prostate carcinomas and still also neuroendocrine tumors. Lutetium and DOTATOC - these are the main therapeutic procedures that we offer. All patients suffering from tumor disease are discussed with all disciplines in an interdisciplinary Tumor Board and we are always present. In my opinion, the tumor board procedure is one of the most important developments in oncology in the last 20 years. In this way, we get to know the patients and their disease history at an early stage and can then decide, together with our colleagues from the other specialties, when such radionuclide therapy should be performed and when it is indicated. This is the usual way patients come "to us."
There are, of course, other ways of direct approach. We are approached directly by the patients or by the treating physicians, and then we also talk to the patient, but the decision for a therapy is always an interdisciplinary joint decision by the tumor board.
-
In Russia, radionuclide therapy is indicated in 50-60% of cancer patients, but according to various estimates, only 10% of patients are actually treated with it. What is the situation in Germany? Was there a breakthrough in the field of radiotherapy in German medicine at a certain point in time?
You really have to relate radionuclide therapy to individual tumors.
I think across all cancer patients, 50% to 60% is certainly too high. In the case of thyroid carcinoma, we are certainly at over 90% of patients who should receive radionuclide therapy; in the case of prostate carcinoma or neuroendocrine tumors in the course of the disease, we also have high percentages. I cannot speak exactly for the situation in Russia; it is always a question of how many therapy facilities are available in a country in order to be able to care for patients nationwide. Here in Germany, we are in the favorable situation of having facilities like ours (in Berlin-Buch) for our patients in practically every federal state, so that we can say that we can make these therapies available to all our patients if they are indicated.
I know that this is different in other countries, and this also leads to the fact that we like to cooperate with colleagues in other countries, especially in Russia, in order to make it possible for patients from there to receive this therapy if it is indicated.
• Please tell us about nuclear medicine diagnostics. To what extent does the PET/CT procedure increase the accuracy of the diagnosis compared to CT or MRI? What other imaging modalities do you use?
This is a very important question. If we stay with tumor diseases, pure CT is actually the standard procedure here. MRI is additionally performed for specific questions, for example, in the case of prostate carcinoma or the presence of liver metastases.
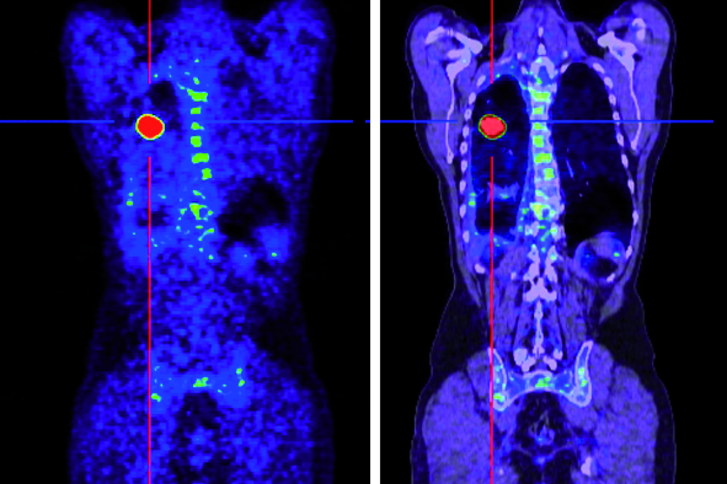
PET/CT is a complementary procedure, it does not replace CT or MRI. We supplement CT with PET (positron emission tomography). This is a functional procedure where we detect metabolism. Here we are able to detect tumor metabolism with high sensitivity, which is not possible with CT or MRI. The combination of PET and CT is particularly charming, because CT of course excellently depicts the anatomy of the patient, PET depicts the metabolism of the tumors, and with both methods together we can detect tumor foci in the patient's body with a very high degree of accuracy and, thanks to the additional information, describe very precisely where this tumor is located and thus describe the environment very precisely to the surgeons, the radiation therapists, thus improving the planning of the radiation therapy and the planning of the operation. The so-called therapy control that we achieve in this way helps our colleagues from other disciplines to simplify the therapeutic procedure.
I mentioned this before, we picture the tumor metabolism and see the patient's entire body. In tumor disease, it is very important to examine the entire body as part of what is called "staging" to see how spread out the tumor disease is.
Let's imagine the following situation:
If a patient not only has a primary tumor, for example a colon tumor, and in addition would already have metastases in the liver and other organs, then the therapy must of course be different than if there is only a colon tumor. In that case, the patient would be operated on first. But if there are already metastases, then perhaps chemotherapy is a better therapy. And you can find all that out exactly with the PET/CT procedure.
And one last aspect to this, which is connected with a new keyword that has become widespread in medicine in recent years. The word is "theranostics", meaning both therapy and diagnostics. Here I could describe the arc again to the already discussed lutetium therapy, because we use the same substance PSMA (prostate carcinoma) or DOTATOC in neuroendocrine tumors, both to perform high-quality diagnostics with PET (there the PSMA is then labeled with gallium or with fluorine), and to perform the therapy with the same substance PSMA (labeled with lutetium). This means that we have the special possibility here of displaying the foci in the patient very precisely with PSMA in PET/CT and then treating these foci directly with the lutetium PSMA and then observing during the course with the aid of PET/CT how well the therapy works and how successful the therapy and the treatment of the patient is.
For me, this is a typical expression of advanced modern medicine, that one treats the tumor disease selectively, highly specifically, and observes it with the same tool in order to then ensure the result of the treatment.
• Among others, you use selective internal radiotherapy (SIRT). For whom is it suitable? What are its advantages? Is it only effective in liver cancer / liver metastases or do you also use it in other cases?
Selective Internal Radiation Therapy (SIRT) is a liver-only therapy. Unlike other radionuclide therapies, which we inject intravenously and which have the advantage of reaching metastases throughout the patient's body, it is different here in the case of SIRT.
In SIRT, in collaboration with interventional radiology, a catheter is inserted directly into the hepatic artery, into the lobe or segment of the liver where a liver tumor is located. And then radioactive beads, which are small resin beads loaded with yttrium-90, can be injected here directly into the liver tumor to treat that liver tumor. The principle of the therapy is that it is confined to the liver. This has the advantage that there are no side effects in the rest of the patient's body, so only the liver is treated.
This already gives an indication: this therapy can only be performed if a tumor disease is only in the liver. If the patient also has metastases outside the liver or if the primary tumor has not been treated there, then SIRT cannot be performed. Basically, there are only 2 clear indications for SIRT:
- Primary liver cell tumors (so-called hepatocellular carcinomas). Here, SIRT is also approved as a therapy. Here, too, we present the patient on an interdisciplinary basis and only then decide whether surgery, chemotherapy, radiotherapy or SIRT is the right procedure.
- Colon carcinomas. If the tumor has already been operated on and if there are metastases only in the liver and not in any other organ of the body, and if the patient has already received chemotherapy and it is no longer effective, then all these factors are considered indications for SIRT. We have also been doing this for many years and have gained a lot of experience with this therapy, which is highly effective and we do it in an interdisciplinary way with the radiologists.
• Please tell us about Xofigo therapy. Bone metastases in patients with prostate cancer usually occur in the 4th stage of the disease. Is radiotherapy a palliative measure in this situation? Or is it possible to cure a patient with bone metastases using this technique? Is Xofigo therapy also used as a preventive procedure?
Xofigo therapy is used exclusively in patients with prostate cancer and bone metastases. Xofigo is a trade name for the radium-223, and that binds to the surface of the structures that are altered as part of the bone metastasis in prostate cancer. Then it's an alpha emitter, internal radiation therapy, somewhat comparable to Lutetium 177 PSMA therapy, but it just doesn't just work on the bone, it works everywhere else as well. Xofigo therapy is an alternative for bone metastases of prostate carcinoma, there are also good studies on this, but this is a palliative therapy. We will not be able to eliminate the metastases with it, but it is an effective therapy to relieve the pain. Many patients with bone metastases in prostate cancer suffer from severe pain that has to be treated with strong painkillers. We can alleviate that with Xofigo therapy. It has to be decided for each individual patient whether Xofigo therapy is the right one or whether Lutetium 177 PSMA therapy would not be more suitable. This is an individual decision that is made for each patient.
• Usually, a physician's specialty refers to a specific group of diseases. Nuclear medicine encompasses several areas that are not linked etiologically, but by treatment techniques. What challenges does this present for you as chief resident of the Department of Nuclear Medicine? Is there more interdisciplinary collaboration in your specialty than in cardiology or orthopedics, for example?
We call ourselves a cross-sectional specialty because we don't just deal with the specific diseases and illnesses here, but can actually offer diagnostic or therapeutic procedures for all specialties. These are not only cancer diseases, which we have already mainly talked about, but of course also cardiology, orthopedics or neurology. We have many good procedures for diagnosing the brain, for example.
That's why we see ourselves as a typical cross-sectional specialty. It is quite important for us to be in daily conversation and communication with our colleagues from other specialties and to be present in the corresponding tumor boards or in other meetings to talk about our procedures there and also to offer them if there are problems in diagnostics or in therapy with the patient.
The particular challenges that come from that are, of course, due to the fact that you have to learn your way around everywhere. Of course, we are not specialists for chemotherapy, for general tumor therapies or for all cardiological or neurological diseases, but we must at least have a basic understanding of what these diseases are, how they are usually diagnosed and treated in order to be able to classify our nuclear medicine procedure in the right place and to know where the possibilities but also the limits of our procedures lie, which we can then discuss with our colleagues from other departments.
• Do you believe that difficult emotional decisions must be made by the patient? What happens if the patient disagrees with the treatment strategy you propose? Is the physician allowed to interfere and persuade or dissuade a patient to make a particular decision? How does that usually work?
Basically, patients are increasingly seeking information through other channels and come to us with certain ideas about the diagnosis and treatment of their disease. Of course, we will never persuade the patient to undergo treatment, but we are, of course, already the patient's advisor and recommend to the patient, on the basis of the international guidelines, on the basis of the discussions and decisions of the Tumor Board, which therapy is the right one at the particular stage of the disease. We explain this to the patient in detail and also give reasons for our opinion. We see time and again that patients say that they do not want certain therapy procedures; patients can also often give good reasons for this!
Of course, these are decisions that we respect and discuss together with the patient and the relatives. We see ourselves as experts who can competently advise patients in this regard. As a matter of principle, we always decide together which therapy is the right one for the patient at the particular stage of the disease.
• There are more and more advocates of alternative medicine who talk about the dangers of chemotherapy and radiation, treat different diseases with homeopathy, and believe that there is a connection between suppressed emotions and cancer. Why do you think people voluntarily abandon the benefits of evidence-based medicine? What can be done to fight against it?
I don't think you have to fight against it at all. Homeopathy and alternative medicine have also had many successes. It is simply important that both practitioners and patients know where the limits of these procedures lie and when one should switch to other procedures or evidence-based medicine, or also when these procedures should be supplemented with the classic evidence-based procedure. This is something that we discuss individually with the patient. We also see it as our task to point out risks when we see the risks when patients focus too much on alternative medical procedures and reject the procedures that we are convinced of according to the current study situation. Here we see ourselves more as advisors to the patient and as those who inform the patient about this and make it clear to the patient where the advantages of the respective therapy procedures lie. The bottom line is that every patient is a responsible citizen and, of course, decides for himself which therapy procedure is to be carried out at which stage of the disease. But we have to inform patients about what is the appropriate therapy procedure according to the current state of science.
• Can you tell us about 2-3 cases from your practice that have particularly stuck in your memory? Have you managed to save a patient in a seemingly hopeless situation?
We see these situations all the time, of course, that we have to convince the patient of something because patients have fears about certain therapies. Patients have heard or read things that may influence their final decision.
We also have a lot of experience with what the side effect profiles of the individual therapies look like, how well the therapies are tolerated or not, what can be done about side effects, because of the high number of patients we care for each year. All of this information is also used for when you need to reassure the patient and help them with the decision-making process. You ask about special experiences, there are actually all the time, because every patient is individually different, but to be told a tumor diagnosis is a severe shock for most patients. "Tumor disease is a terrible disease that may lead to death" - that is usually the patient's first opinion. We then try to show in a differentiated way that it is quite different depending on the disease itself and the stage of the disease.
Let me come back to thyroid cancer: yes, it is a cancer and it is a malignant disease, but with a very good prognosis! Well over 90% of patients can be cured. We explain to the patient that surgery is absolutely necessary, that we do radioiodine therapy to achieve further safety, and that it is a combination of both procedures that shows good results. Most of the time the prognosis is so good that after the therapy it looks as if the patient never had this disease at all.
This information helps us to take away the patients' fears. Then, after processing this disease, the patients can definitely learn to process this disease with psychosocial component and also continue your life with good courage. This is also possible with metastasized thyroid carcinoma, to produce healing and to give a good prognosis to a patient with such a disease.
• How did your work change during the pandemic?
Here we have to consider the different phases of the pandemic.
In the initial phase, that is, in the first wave, there was great uncertainty everywhere. Patients were very worried that they might contract SARS-Cov2 just in the hospital, whereas we have never seen the risk higher. On the contrary, in the hospital, many tests are constantly performed on the staff and on the patients. But the fear was there; we had such an impression that many follow-up examinations and also diagnostic and therapeutic procedures were delayed and that patients arrived later. That then changed. After the first wave, many patients were vaccinated, information was better disseminated, and people have already learned a bit how to deal with this pandemic.
Today, for example, with fourth wave in Germany and with high incidence number, we are not limited for our specialty at the moment.
Since we deal a lot with cancer patients, we also tell our patients to continue to come for the necessary examinations or follow-up appointments because we don't want the treatment and diagnosis of such a disease to be delayed. That's where we have simply learned, both we as practitioners and the patients, to deal with this situation. With the necessary protective measures, which we strictly adhere to, also in our direct dealings with our patients, we continue to offer the necessary procedures here.
Personal questions
• Do you currently participate in any studies or research projects? Can you tell us about any promising discoveries or perspectives in your area?
Research projects or studies are something that is always important to us and something that I have pursued intensively in my professional life and partly during my studies. Scientific work is an interesting additional aspect of our profession. At the moment we are focusing on an exciting topic "the brain", which I am now personally very interested in. Furthermore, dementia, Alzheimer's disease, diseases of the brain, is also important for the populations of all countries. Here, too, we have the modern PET-CT diagnostic procedure with new substances whose therapeutic effects we can check in the course of a disease; here we have been participating in scientific studies for many years, in collaboration with our colleagues from neurology and psychiatry. This is really a highly interesting field where, if the results are good, patients from all over the world could benefit. Anyone who can observe a patient with dementia knows how much of a burden it is for the patient and for their family. Our aging society has clearly shown us that these scientific projects are important and relevant right now.
You also asked about the prospects - especially in the area of dementia and Alzheimer's disease, there are many companies that are working on the therapeutic substances that we can then study with PET CT as we go along. The other thing is, in terms of oncology. We think that Lutetium PSMA therapy is just the beginning of new developments in our field. We know that there are various other substances in development, some of which are already in initial clinical trials, both for diagnostics and for therapy; here I come back to the keyword theranostics. These substances will certainly be available in the near future and can also be used in a similar way, such as PSMA therapy for prostate cancer, for other cancers.
• What do you find most valuable about your work? What is the greatest challenge?
Nuclear medicine is a small specialty, but it can provide very important components of patient care in both diagnostics and therapy for certain diseases. That is the beauty of being able to provide comprehensive care for patients with these kinds of issues.
I would also mention another aspect: there is generally the care of patients with thyroid tumor diseases. This shows that our specialty is a typical cross-sectional area, because we also care for patients here like a general practitioner. We regularly have our consultation hours always related to the thyroid diseases on site, we perform examinations and treatments over years and decades. And this makes our small specialty so comprehensive that it is very satisfying for us as physicians and brings joy to our work.
• How did you decide to become a physician? Why did you choose nuclear medicine? Does working in this specialty require certain personal or character traits?
I have always been interested in the natural sciences and that was also part of the Abitur. Studying pure natural sciences then seemed too theoretical to me, and so I came to medicine, which I liked very much from the beginning. I actually came to nuclear medicine by chance: at the time when I started working in medicine, in the mid-1990s, the subjects of radiology, radiation therapy and nuclear medicine were combined at the large hospitals and at the university in Munich where I started. I started in radiology and did services in radiotherapy, and then was in nuclear medicine as part of that rotation. The subject at that time didn't mean that much to me, because at that time during my studies this subject had been treated very lightly. However, I liked it very much, especially this combination of diagnostics and therapy. After 1.5 years, I decided to focus on nuclear medicine and have not regretted it to this day. The work is a lot of fun.
• Do you believe that the profession of medicine is primarily a talent? Or is it rather a set of skills and knowledge that anyone can acquire?
This is, I think, a combination of the things mentioned: character, talents, skills and knowledge, but also, of course, the personal characteristics of the person. Of course, it's not just limited to medicine, because as people we develop significantly over the years and our skills and expertise are always expanding. How we interact with our patients, how we care for the patient, how we respond to patients and family members - all of this is an evolving process in our profession that never comes to a halt. These processes are also part of the job description.
• Do you keep in touch with your patients?
Yes, mostly (but not exclusively) with the thyroid patients we see and follow up with here regularly over decades. And again, we have ongoing contact through contacts who also coordinate other treatment needs and build a long-term patient relationship.
But also with the other therapy methods such as Lutetium PSMA therapy, it is the case that the therapy is not carried out once, but in several cycles of several weeks to months, so that we also care for these patients over a longer period of time together with the urologists, with the oncologists and with the other attending physicians.
This is also part of our job description, to have contact with a patient not only for a short time, but to accompany the patient over a longer period of time.
• How do you spend your free time?
Of course, this is very different and depends on the season! We have talked about many difficult topics today and also about seriously ill people, and of course, at the end of the day, doctors need to find a balance and nurture your own interest.
In the Summer I prefer sporting activities outside, and in the Winter quite differently. We have such a huge range of options here in Berlin, and we are constantly trying to do something with my wife and get our minds off things after the workday.
Read more:
-
Helios Hospital in Berlin Buch offers MIBG Therapy: treatment of advanced-stage neuroendocrine tumor
-
Diagnosis and therapy for prostate cancer with Lutetium-177 PSMA–DKFZ 61
-
About Helios Hospital Berlin Buch